Introduction
A mood disorder recognized through not severe symptoms like depressive episodes and hypomanic. These are still comparatively less severe when compared to bipolar disorder. This is known as cyclothymia. In order to meet the diagnostic criteria, the signs must be noticed for at least two years for an adult. Additionally, a year for children or teens.
What are Cyclothymia Therapies?
Cyclothymia can be treated in various ways, initiating from a proper diagnosis. It is essential for the mental health professional to conduct a physical exam first to eliminate differential diagnoses. Following that, based on the symptomatology, the professional conducts a complete psychological evaluation along with mood charting.
Once the diagnosis is final, the treatment approach depends on the level of dysfunction caused by cyclothymia. In case the onset is recent with mild to moderate impact, the focus is on the prevention of bipolar disorder and other comorbidities. This involves reducing the frequency and severity of symptoms, prevention of relapse, and treatment for substance use problems.
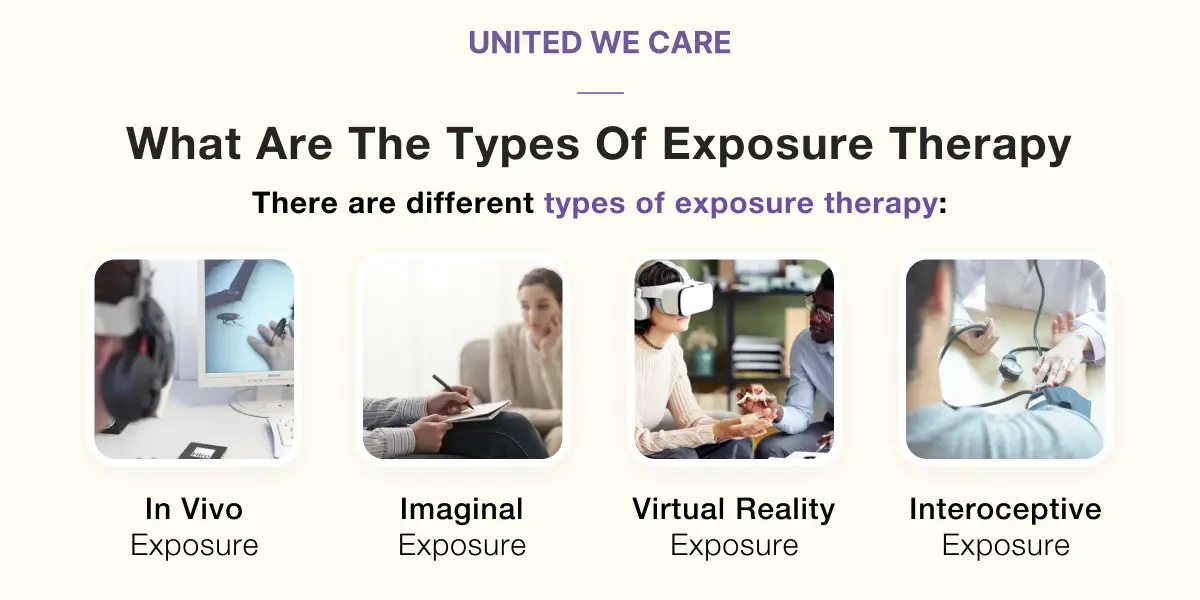
Typically, cyclothymia is treated with a multi-modal approach. Generally, this includes the use of medication, CBT, interpersonal and social rhythm therapy, and other individualized therapies varying from case to case.
Application of Cyclothymia Therapies
Before one may begin to apply cyclothymia therapies, it is important for the client and therapist to collaborate in their therapeutic alliance. They must come to a consensus to figure out the source they want to use to connect the therapy with.
From one perspective, this may seem like a hierarchical approach. Firstly, the therapist works with the client to decide which area of symptoms they want to tackle. Usually, this includes relatively less severe or mixed depressive episodes. Eventually, they work their way towards comorbidities and other severe symptoms.
Moreover, the mechanism works with a mid-term goal of a period of 6-12 months. This is a period that focuses on preventing extreme episodes and simply mood stabilization initially. Additionally, as the depth of the therapeutic alliance increases, long-term goals begin to emerge.
This may involve fixing dysfunctional schemas, functional recovery, and coping skill development. It is common for professionals to introduce medication at this stage of therapy to buttress the psychotherapeutic work being conducted. Lastly, it is of great advantage if the client grows to become more aware and accepting of their condition.
Efficacy of Cyclothymia Therapies
Cyclothymia therapy is significant when it comes to seeing its effect.
- The researchers have figured that lithium, valproate, and lamotrigine are some mood stabilizers. Also, they help the patient deal with mood episodes and reduce them.
- Apart from this, antidepressants are capable of making the symptoms worse. Additionally, these should only be considered when the patient is looking for a short-term treatment.
- If not treated the right way and through tailored procedures for help, it might present worsening symptoms. So, while trying to figure out what works the best, studies have also found some special results.
- Patients have been able to see results through cyclothymia-focused psychoeducation groups as well.
- Along with this, at this time, if one adopts medication and psychotherapy with a plan, it might actually help a lot. Furthermore, these two associated together show very practical improvement in the nature of therapy.
Where to Find Cyclothymia Therapies?
Importantly, to start with cyclothymia treatment, one must figure out the source they want to use to connect with it.
Psychiatrist or Mental health Professional
So, in order to first diagnose oneself, a psychiatrist or mental health professional can help and treat it further. In order to recognize an issue, one must acknowledge it.
Medications
Apart from this, when one starts with medications, the prescriptions and their impact are usually kept under a healthcare provider’s supervision.
Psychotherapy
In addition, for influential psychotherapy, one must refer to psychologists, counselors, and even social workers who have relevant knowledge.
Online resources
Not only this, a virtual mode of treatment is also available to implement cyclothymia therapy at one’s convenience. Online support groups and other online resources present the patient with an opportunity to connect with others with cyclothymia. It should also be noted that psychoeducation groups focused on treatment are also reachable through the Internet.
Conclusion
Hence, cyclothymia might be just a mild mood disorder, but it requires a deep understanding of the treatment. Along with this, one must be accompanied by the procedure of psychotherapy and the mechanism of medications. This helps with implementing the strategies of the treatment process.
It should be noted that the hierarchical approach involves dealing with impairing issues and, later, mood stabilization. Its efficacy can also be observed through mood stabilizers, impactful psychotherapy, and the attached risks of antidepressants. This treatment asks for a commitment to it in order to see the results. Last but not least, cyclothymia therapy treats and prevents progress in the disorder itself. Also, it features practical recovery in order to help the patient.
References
- American Psychiatric Association, “Diagnostic and Statistical Manual of Mental Disorders: DSM-5,” Arlington, VA: American Psychiatric Publishing, 2013.
- J. Angst and A. Marneros, “Bipolarity from ancient to modern times: Conception, birth and rebirth,” Journal of Affective Disorders, vol. 67, pp. 3–19, 2001.
- G. S. Malhi and E. Bell, “Schizoaffective disorder: A ‘dysfunctional’ proposal?” Bipolar Disorders, vol. 21, pp. 298–301, 2019.
- G. Perugi et al., “The bipolar-borderline personality disorders connection in major depressive patients,” Acta Psychiatr. Scand., vol. 128, no. 5, pp. 376–383, 2013. [PMID: 23379930].
- G. Domes, L. Schulze, and S. C. Herpertz, “Emotion recognition in borderline personality disorder-a review of the literature,” J. Pers. Disord., vol. 23, no. 1, pp. 6–19, 2009. [PMID: 19267658].
- A. C. Ruocco et al., “Neural correlates of negative emotionality in borderline personality disorder: an activation-likelihood-estimation meta-analysis,” Biol. Psychiatry, vol. 73, no. 2, pp. 153–160, 2013. [PMID: 22906520].
- G. Delvecchio, G. Sugranyes, and S. Frangou, “Evidence of diagnostic specificity in the neural correlates of facial affect processing in bipolar disorder and schizophrenia: a meta-analysis of functional imaging studies,” Psychol. Med., vol. 43, no. 3, pp. 553–569, 2013. [PMID: 22874625].