Introduction
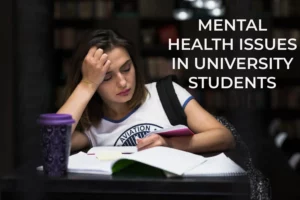
Post-traumatic stress disorder (P.T.S.D.) is a psychological disorder that affects individuals who experience death, sexual violence, or significant injury. In addition, a person who has experienced or witnessed an event such as a severe accident, a natural disaster, a war/combat, terrorist attack, rape, violence, etc., which is traumatic, can also be diagnosed with P.T.S.D.
Our Wellness Programs
What is P.T.S.D.?
People who suffer from P.T.S.D. have vivid, unsettling thoughts and sensations about the traumatic incident that last long after. The patients have flashbacks or nightmares about the occurrence and may experience sadness, fear, rage, and a sense of separation from their loved ones.
Persons with P.T.S.D tend to avoid the people, situations, and circumstances that remind them of the unpleasant experience. They may strongly react to seemingly innocuous things like a loud noise or an unintentional touch.
Traumatic experiences trigger post-traumatic stress disorder or P.T.S.D; however, the exposure could be indirect rather than first-hand. For example, a person who learns about the death of a family member may also be diagnosed with P.T.S.D. It can also happen due to frequent exposure to gruesome details of the trauma, such as police personnel exposed to child abuse case specifics.
Looking for services related to this subject? Get in touch with these experts today!!
Experts

Kirti Bajpai

India
Psychologist
Experience: 5 years

Neelam Parwani

India
Life Coach
Experience: 5 years

Mansi Chawla

India
Psychologist
Experience: 12 years
Why is P.T.S.D. common in Veterans (ex-military personnel)?
The harsh working conditions expose military personnel to various traumas that civilians do not experience because of the frequent trauma during wartime, high risk of the service, and stress. Additionally, deployment to a war zone, training accidents, and military sexual trauma (or M.S.T.) are the main reasons a veteran is more likely to be diagnosed with P.T.S.D.
After experiencing significant trauma or a life-threatening event, one may develop post-traumatic stress disorder (P.T.S.D.), also known as shell shock or combat stress. It’s natural for your mind and body to be in shock after a traumatic experience, but when your nervous system reacts or becomes “stuck,” that is called P.T.S.D.
What are the symptoms of P.T.S.D. common in Veterans (ex-military personnel)?
While P.T.S.D. Symptoms might appear within hours or days of a stressful experience; symptoms may not appear for a few months or even years after the individual returns from deployment.
While each veteran’s P.T.S.D. Manifests as there are around four symptom clusters to look for:
- Intrusive reminders of the traumatic incident, such as distressing nightmares, thoughts, and flashbacks in which you believe the experience is repeating itself. And these reminders are recurrent. Panic attacks, uncontrollable shivering, and heart palpitations are examples of intense reactions (physical and emotional) to trauma memories.
- Extreme aversion to everything reminds the traumatic experience and triggers terrible memories of places, thoughts, people, or events. Losing interest in routine activities and being withdrawn from family are examples of this.
- Exaggerated negative ideas and persistent feelings of humiliation, guilt, and fear are examples of unfavourable alterations in their thoughts and attitude. They might notice a decrease in your ability to feel happy.
- Some symptoms of P.T.S.D are irritability, rage, reckless behaviour, difficulty sleeping, and lack of concentration.
What are the effects of P.T.S.D. common in Veterans (ex-military personnel)?
Some common effects of P.T.S.D. among veterans include:
- Intrusion: Thoughts, such as involuntary memories, disturbing nightmares, or flashbacks to the traumatic incident are examples of intrusion. Intense flashbacks make the sufferer believe that they are reliving the painful event.
- Avoidance: Avoiding people, places, activities, items, and situations that may remind of the upsetting memories of the traumatic incident. People strive to avoid recalling or forgetting the traumatic event and would also feel not to discuss it.
- Alterations in cognition and mood: Inability to recall the details of the traumatic event and feeling distorted about oneself or others. Distorted ideas about the event’s cause are incorrectly blaming oneself or others, much less interest in previously enjoyed activities, feeling detached from others, or inability to experience positive emotions.
- Alterations in arousal and reactivity: Having furious outbursts and feeling irritated; behaving recklessly or in a self-destructive manner; or having trouble concentrating or sleeping are some examples of arousal and reactive symptoms.
What is the treatment of P.T.S.D. common in Veterans (ex-military personnel)?
Some common treatment options for the veterans diagnosed with P.T.S.D. are as follows:
- Cognitive Processing Therapy: Because of the trauma, Cognitive Processing Therapy focuses on altering uncomfortable negative feelings and beliefs. Therapists assist the individual in confronting such upsetting memories and emotions.
- Prolonged Exposure Therapy: To help a person’s face and acquire control of anxiety and discomfort, Prolonged Exposure Therapy involves repeated, detailed imaginations of the trauma or gradual exposures to symptom “triggers” in a safe, controlled fashion. Virtual reality programs have helped reshape how P.T.S.D patients experience the battlefield.
- Stress Inoculation Therapy: This therapy exposes individuals to lower amounts of stress, which helps them develop the proper coping abilities against stressful triggers. This process is similar to how a vaccination prevents infection following exposure to an illness.
- Group therapy allows survivors of similar traumatic events to discuss their feelings and experiences in a safe, non-judgmental environment. Members of the group assisted one another in realising that many others would have reacted similarly and had the same emotions. Because the behaviour and misery of the person with P.T.S.D. can impact the complete family, counselling for the whole family may prove beneficial.
Conclusion
Some soldiers develop P.T.S.D. while others don’t; the risk of developing P.T.S.D. is unknown. It may depend upon the number of tours and combat experiences veterans encounter during their tenure. Soldiers may experience hypervigilance, hyperawareness, and adrenaline-quick reflexes. It becomes inappropriate when the veteran returns home.
Thus, learning how to “unstuck” takes time, and you will learn the process gradually. But if you cannot overcome the stress, you have a high chance of being diagnosed with P.T.S.D.
Some common symptoms of P.T.S.D. are reckless behaviour, the occurrence of opposing ideas, and others. Symptoms must endure for more than a month and create significant distress or difficulty in the individual’s everyday functioning to be diagnosed with P.T.S.D. Depression, substance abuse, memory problems, and other physical and mental health issues are common co-occurring illnesses with post-traumatic stress disorder.